|
What is Breast Cancer?
Common Symptoms
What Causes Breast Cancer?
Treatments
After Treatment
Additional Information
What is Breast Cancer?
Breast cancer is the most common cancer occurring in women (excluding
cancers of the skin) and the second most common cause of death from cancer in
women after lung cancer. Men can also develop breast cancer, but male breast
cancer is rare, accounting for less than 1% of all breast cancer cases. If
diagnosed at an early stage, breast cancer has an encouraging cure rate: up to
97% of women diagnosed with localized breast cancer will survive five years
after their diagnosis. Even if the cancer is found at a more advanced stage, new
therapies have enabled many people with breast cancer to experience a good
quality of life.
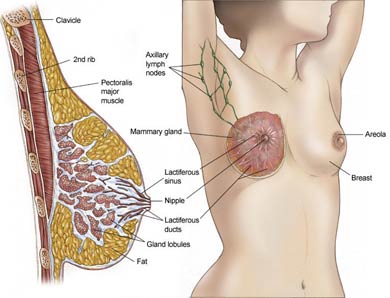
The breast is comprised mainly of fatty tissue. Within this tissue is a network
of lobes, which are made up of tiny, tube-like structures (called lobules) that
contain milk glands. Tiny ducts connect the glands, lobules, and lobes and carry
the milk from the lobes to the nipple, located in the middle of the areola
(darker area that surrounds the nipple of the breast). Blood and lymph vessels
run throughout the breast; blood nourishes the cells, and the lymph system
drains bodily waste products.
The main forms of breast cancer are:
- Invasive ductal carcinoma — This type of breast cancer develops
in the milk ducts and accounts for about 79 percent of cases. It can break
through the duct wall and invade the breast's fatty tissue, then metastasize
(spread) to other parts of the body through the bloodstream or lymphatic system.
- Invasive lobular carcinoma — This type of breast cancer
accounts for about 10 percent of cases and originates in the breast's
milk-producing lobules. It also can spread to the breast's fatty tissue and
other places in the body.
- Medullary, mucinous and tubular carcinomas — These are three
slow-growing types of breast cancer. Together they represent about 10 percent of
all breast cancers.
- Paget's disease — This type represents about 1 percent of
breast cancers. It starts in the milk ducts of the nipple and can spread to the
areola (dark circle around the nipple). Women who get Paget's disease usually
have a history of nipple crusting, scaling, itching or inflammation.
- Inflammatory carcinoma —This type accounts for about 1 percent
of all cases. Of all breast cancers, inflammatory carcinoma is the most
aggressive and difficult to treat, because it spreads so quickly.
- Ductal carcinoma in situ (DCIS) — DCIS occurs when cancer cells
fill the ducts but haven't yet spread through the walls into fatty tissue.
Nearly all women diagnosed at this early stage can be cured. Without treatment,
about 25 percent of DCIS cases will lead to invasive breast cancer within 10
years.
- Lobular carcinoma in situ (LCIS) — LCIS is less common and less
of a threat than DCIS. It develops in the breast's milk-producing lobules. LCIS
doesn't require treatment, but it does increase a woman's risk of developing
breast cancer.
Common Symptoms?
A woman who has breast cancer may have no problems, or she may find a painless
lump in her breast. If women examine their breasts monthly, they can help find
lumps or other changes that a doctor should examine.
Most breast lumps are not cancer, but all lumps should be checked out by a
doctor to be sure. Non cancerous breast lumps may be scar tissue or cysts
(fluid-filled lumps or sacs) or they can be due to normal breast changes
associated with hormone changes or aging.
Symptoms of breast cancer include:
- A lump or thickening in the breast or under the arm
- A clear or bloody discharge from the nipple
- Persistent crusting or scaling of the nipple
- Inverted nipples
- Redness or swelling of the breast
- Dimpling on the breast skin resembling the texture of an orange
- A change in the contours of the breast, such as one being higher than the other
- A sore or ulcer on the skin of the breast that does not heal
What Causes Breast Cancer?
Many cases of breast cancer occur in women with no obvious risk factors. This
means that women need to be alert in watching for possible changes in their
breasts, performing self-examinations, and scheduling clinical breast
examinations and mammograms. It is likely that multiple risk factors influence
the development of breast cancer. Some of these include:
Age. The risk of developing breast cancer increases as a woman
ages, with the majority of breast cancers developing in women over the age 50.
At age 30, a woman's risk of developing breast cancer is one in 2,525. By age
50, her chances are one in 50, rising to one in 14 by age 70.
Race. Although white women are more likely to develop breast
cancer, black women are more likely to die from the disease. The reasons for
this are unclear and probably involve both socioeconomic and biologic factors.
Previous history of breast cancer. Women who have had breast
cancer in one breast have three to four times the risk of breast cancer in their
opposite breast.
A history of endometrial or ovarian cancer. The development of
these cancers is also associated with exposure to hormones and, therefore, a
woman's risk of breast cancer may also be increased. Some BRCA1 or BRCA2 gene
mutations may also increase the risk of both ovarian and breast cancers.
A family history of breast cancer. Women who have a
first-degree relative (mother, sister, daughter) diagnosed with breast cancer
are at increased risk of the disease. More than one first-degree relative with
breast cancer elevates that risk.
A genetic predisposition. Mutations to the BRCA1 or BRCA2 genes
are associated with increased breast cancer risk. Screening tests are available
to test for known mutations to these genes, but are not recommended for everyone
and only following appropriate genetic counseling. Researchers estimate that
breast cancers caused by these genes make up only 2% to 3% of all breast
cancers.
Estrogen exposure. Estrogen is a hormone in women that controls
the development of secondary sex characteristics (such as breast development). A
woman's production of estrogen decreases at menopause. Doctors think that
exposure to estrogen for a long time may increase breast cancer risk:
- A long menstrual history: Women who began menstruating before age 12 or went
through menopause after age 55 have a higher risk of breast cancer because their
breast cells have been exposed to estrogen for longer periods of time.
- Late or no pregnancies: Women who have their first pregnancy after age 30 or who
have never had a full-term pregnancy have a higher risk of breast cancer.
Pregnancy may protect against breast cancer because it pushes breast cells into
their final phase of maturation.
- Estrogen in medication: Recent use of oral contraceptives or hormone replacement
therapy (HRT), or long-term use of HRT, may increase a woman's risk of breast
cancer.
Atypical hyperplasia. This is a condition characterized by
abnormal, but not cancerous, cells. Atypical hyperplasia is a risk factor of
breast cancer.
Lobular carcinoma in-situ. This is associated with an increased
risk of developing a cancer in either breast when found within an otherwise
benign breast biopsy.
Lifestyle factors. As with other types of cancer, studies
continue to show that various habits may contribute to the development of breast
cancer. These include:
- Obesity: According to a new study, being obese or even overweight increases a
woman's risk of breast cancer.
- Lack of exercise: Exercise lowers hormone levels and boosts the immune system;
lack of exercise contributes to obesity.
- Alcohol use: Drinking more than one alcoholic drink per day may raise the risk
of breast cancer.
Radiation. High doses of radiation may increase a woman's risk
of breast cancer. An increased risk of breast cancer has been observed in
long-term survivors of atomic bombs, patients with lymphoma treated with
radiation therapy to the chest, patients undergoing large numbers of x-rays for
tuberculosis or non-malignant conditions of the spine, and children treated with
radiation for tinea capitis (ringworm).
Treatments for Breast Cancer
Even though the doctor will tailor the treatment for breast cancer to the
patient's disease and personal situation, there are some general steps in the
logic of treating the disease. Primarily, the initial therapy for early stage
disease is aimed at eliminating any visible tumor. Therefore, doctors will
recommend surgery to remove the tumor with or without radiation therapy.
The next step in the management of early stage disease is to reduce the risk of
the disease recurring and to eliminate any cancer cells that may remain. If a
tumor is of a certain size or lymph nodes are involved, the doctor may recommend
additional therapy, such as radiation therapy, chemotherapy, or hormonal
therapy. If the cancer recurs, the patient may choose additional surgery,
depending on where the cancer is found, or a variety of treatments designed to
fight distant metastases.
Surgery
Generally, the smaller the tumor, the more surgical options a patient has. The
general types of surgery include the following:
- Lumpectomy - A lumpectomy removes the tumor and a small
"clean," or disease-free, margin of tissue around the tumor. Follow-up radiation
therapy is given to the disease site.
- Partial Mastectomy - A partial mastectomy removes the tumor, an
area of normal tissue, and part of the lining over the chest muscle where the
tumor was. This surgery is similar to a lumpectomy. It is also called a
segmental mastectomy and requires follow-up radiation.
- Modified Radical Mastectomy - A modified radical mastectomy
removes the breast, some of the underarm lymph nodes, and the lining over the
chest muscles.
- Total Mastectomy - A total mastectomy removes the entire
breast, leaving the underarm lymph nodes intact. This surgery is also called
simple mastectomy.
- Radical Mastectomy - A radical mastectomy removes the breast,
chest muscles, all lymph nodes under the arm, and additional fat and skin. It
used to be the standard surgical treatment for breast cancer, but is an uncommon
procedure today. About 15% of women who have had radical mastectomies experience
lymphedema, the buildup of fluid in the lymph system.
Women are encouraged to talk with their doctors about which surgical option is
right for them. More aggressive surgery is not always better and may result in
additional complications.
Choosing Between Lumpectomy and Mastectomy
One advantage of lumpectomy is that it saves the way the breast looks.
A downside is the need for several weeks of radiation after surgery. But some
women who have a mastectomy will still need radiation. For most women with stage
I or II breast cancer, lumpectomy or partial mastectomy (along with radiation)
is as good as mastectomy. There is no difference in the survival rates of women
treated with these 2 methods. Other factors, though, can affect which type of
surgery is best for you. And lumpectomy is not an option for all women with
breast cancer. Your doctor can tell you if there are reasons why a lumpectomy is
not right for you.
Possible side effects of mastectomy and lumpectomy include infection and blood
or fluid collecting at the place where the incision is made. If lymph nodes are
removed, there could be other side effects as well such as swelling of the arm
(lymphedema).
Radiation Therapy and Chemotherapy are often used after
lumpectomy or mastectomy to make sure that all the cancer cells are destroyed
and do not grow back.
- Radiation therapy almost always is recommended after lumpectomy to destroy any
cancer cells left behind and to prevent the cancer from returning. Without
radiation therapy, the odds of the cancer returning increase by about 25
percent.
- The need for Chemotherapy depends on how much the cancer has spread. In some
cases, chemotherapy will be recommended before surgery to shrink a large tumor
so that it can be removed more easily. Chemotherapy is almost always necessary
if cancer recurs. A form of chemotherapy called hormonal chemotherapy usually is
recommended when the pathology report shows that the cancer is estrogen-receptor
positive.
After Treatment
After the first course of treatment is finished, it is very important to keep
all follow-up visits to your doctor. Be sure and tell the doctor about any
symptoms or side effects that concern you.
Lymphedema is a swelling of the arm caused by fluid build up that may occur
after treatment for breast cancer. It's hard to tell which women will develop
lymphedema. It can happen right after surgery, or months or even years later.
With care, lymphedema can often be avoided or kept under control. Injury or
infection of the arm on the affected side can cause lymphedema or make it worse.
Tell your doctor right away about any swelling, tightness, or injury to the hand
or arm. There are ways to help prevent problems. More information about
lymphedema is available through our toll-free number or on our Web site.
Treatment for breast cancer can affect the pleasure from touching the breast. In
a reconstructed breast, the feeling of pleasure from touching the nipple is
largely lost because a preserved or rebuilt nipple has much less feeling than a
natural one. The skin of the breast itself may be less sensitive, too. Some
feeling can return after time, though.
About Breast Forms and Bras
Some women who have had a mastectomy might choose breast forms instead
of reconstruction. Your doctor will tell you when you are ready to be fitted for
a permanent form. Prices of forms vary quite a bit. Take time to shop for one
that looks good and fits well.
The right bra for you may very well be the one you have always worn. You can
often have your usual bra adapted for a breast form. Be sure to check your
insurance to see what is covered and how to file a claim. Also, ask your doctor
to write prescriptions for your form and any special bras. When buying the forms
or bras, have the bills marked "surgical."
Be aware that if you submit an insurance claim for a form or a bra, the company
might not also cover reconstruction if you decide you want this procedure in the
future. Get all the facts before turning in any claims.
Pregnancy
In the past, many doctors advised breast cancer survivors not to become
pregnant for at least 2 years after treatment. Although only a few studies have
been done, nearly all have found that pregnancy does not increase the risk of
the cancer coming back after successful treatment. If you are thinking about
getting pregnant, be sure to discuss the issue with your doctor. Sometimes
counseling can help you sort out the complex issues about motherhood and breast
cancer survivorship.
Additional Information
National Organizations and Web Sites
Encore Plus Program of the YWCA
Office of Women's Health Initiatives
Telephone: 800-953-7587 or 202-467-0801
Call to find a program in your area.
National Breast Cancer Coalition
1101 17th Street, NW, Suite 1300Washington, DC 20036
Telephone: 800-622-2838 or 202-296-7477
Internet Address:
www.natlbcc.org
National Cancer Institute (NCI)
Telephone: 1-800-4-CANCER
Internet Address: www.cancer.gov
Susan G. Komen Breast Cancer Foundation
Telephone: 800-IM-AWARE or 1-800-462-9273
Internet Address: www.komen.com
Y-ME National Breast Cancer Hotlines
Telephone: 1-800-221-2141 (English), 1-800-986-9505
(Spanish)Internet Address:
www.y-me.org
Centers for Disease Control and Prevention (CDC) DES Update
Telephone: 1-888-232-6789
Internet Address:
www.cdc.gov/des
|